Emerging research is painting an alarming picture of how Covid and the Covid vaccines stand to negatively impacting the health of nearly all of us.
Researchers say one of the biggest issues lies in the unique “spike protein” of Covid, which the vaccines instruct our bodies to make.
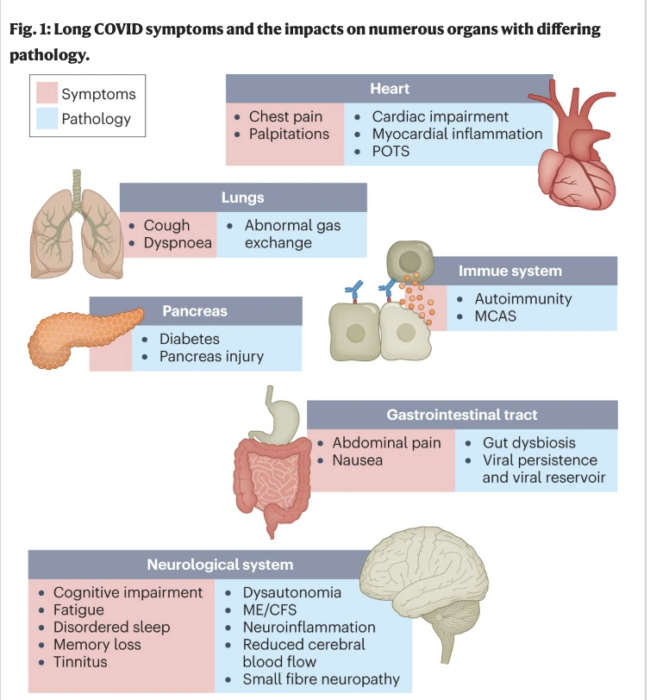
There is a wide array of symptoms that sometimes emerge seemingly out of the blue months or years later, even among those who had no symptoms of Covid at the time, or suffered no obvious immediate adverse events from the vaccine. They include critical tissue damage and problems with heart, lungs, skin, blood, endocrine system, kidneys, brain, liver, gastrointestinal system and more.
Scientists say this could manifest as clots, stroke, heart issues including atrial fibrillation, shortness of breath, extreme tiredness and/or weakness, paralysis, thinking problems, and more.
According to researchers, your regular specialists may not recognize the link to a Long Vax or Long Covid illness for several reasons. First, they aren’t being taught the emerging science on the topics, and the government certainly isn’t spending any serious effort to push it out. Second, some of the problems, such as microclots, are not observable through the normal scans and diagnostic tests that doctors typically rely upon. Third, if the physicians can attribute the illness to any other cause, such as aging or pre-existing conditions, they often write it off and don’t understand the need to dig more deeply.
The reason to dig more deeply has to do with the fact that researchers say Long Vax and Long Covid can potentially be treated. Clinicians are experimenting with various therapies. The treatments may look quite different from the ordinary therapies doctors are used to prescribing.
The following study has quite a bit of information on Long Covid (which also applies to Long Vax, according to researchers, even though vaccines are not always mentioned in the same context).
Abstract
Long COVID is an often debilitating illness that occurs in at least 10% of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections. More than 200 symptoms have been identified with impacts on multiple organ systems. At least 65 million individuals worldwide are estimated to have long COVID, with cases increasing daily. Biomedical research has made substantial progress in identifying various pathophysiological changes and risk factors and in characterizing the illness; further, similarities with other viral-onset illnesses such as myalgic encephalomyelitis/chronic fatigue syndrome and postural orthostatic tachycardia syndrome have laid the groundwork for research in the field. In this Review, we explore the current literature and highlight key findings, the overlap with other conditions, the variable onset of symptoms, long COVID in children and the impact of vaccinations. Although these key findings are critical to understanding long COVID, current diagnostic and treatment options are insufficient, and clinical trials must be prioritized that address leading hypotheses. Additionally, to strengthen long COVID research, future studies must account for biases and SARS-CoV-2 testing issues, build on viral-onset research, be inclusive of marginalized populations and meaningfully engage patients throughout the research process.
Introduction
Long COVID (sometimes referred to as ‘post-acute sequelae of COVID-19’) is a multisystemic condition comprising often severe symptoms that follow a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection. At least 65 million individuals around the world have long COVID, based on a conservative estimated incidence of 10% of infected people and more than 651 million documented COVID-19 cases worldwide1; the number is likely much higher due to many undocumented cases. The incidence is estimated at 10–30% of non-hospitalized cases, 50–70% of hospitalized cases2,3 and 10–12% of vaccinated cases4,5. Long COVID is associated with all ages and acute phase disease severities, with the highest percentage of diagnoses between the ages of 36 and 50 years, and most long COVID cases are in non-hospitalized patients with a mild acute illness6, as this population represents the majority of overall COVID-19 cases. There are many research challenges, as outlined in this Review, and many open questions, particularly relating to pathophysiology, effective treatments and risk factors.
Hundreds of biomedical findings have been documented, with many patients experiencing dozens of symptoms across multiple organ systems7 (Fig. 1). Long COVID encompasses multiple adverse outcomes, with common new-onset conditions including cardiovascular, thrombotic and cerebrovascular disease8, type 2 diabetes9, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)10,11 and dysautonomia, especially postural orthostatic tachycardia syndrome (POTS)12 (Fig. 2). Symptoms can last for years13, and particularly in cases of new-onset ME/CFS and dysautonomia are expected to be lifelong14. With significant proportions of individuals with long COVID unable to return to work7, the scale of newly disabled individuals is contributing to labour shortages15. There are currently no validated effective treatments.
Visit The Sharyl Attkisson Store today
Unique gifts for independent thinkers
Proceeds benefit independent journalism








